NORMAL CIRCULATION
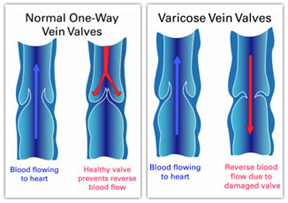
Healthy arteries and veins act as ‘one-way streets’, allowing blood to flow in one direction only. The beating heart directs blood through arteries to the entire body. Blood is then returned to the heart through the veins. The contraction of the leg muscles acts like a pump to move blood up the veins, against the force of gravity. The one-way valves in the leg veins prevent the backflow of blood down towards the feet.
There are two systems of veins: deep and superficial. Deep veins are located well below the skin, often within the muscles, and are crucial in maintaining a healthy circulation. Superficial veins are located near the skin surface, and drain into the deep veins through junctions. Superficial veins are also connected to deep veins through multiple small connections called ‘perforating veins’. Valves inside the perforating veins and junctions prevent the flow of blood back into the superficial veins. Blood thus naturally flows from the superficial veins into the perforating veins and junctions, which connect to the deep veins and then back to the heart.
Saphenous veins are the main superficial veins in the legs. Saphenous veins collect blood from other surface veins and drain it into the deep veins. The longest, the Great Saphenous Vein, is located in the inner aspect of the leg and travels from the ankle to the groin. The Small Saphenous Vein is located at the back of the calf muscle and travels from the outer ankle to the back of the knee. The Great Saphenous Vein is the vein that is most commonly ‘stripped’ in varicose vein operations.
ABNORMAL VEINS
Abnormal veins have weak walls. These veins collect and contain more blood than normal veins, causing distension in the vein. Because of this distension, the valves no longer function properly, which causes a ‘leakage’, ‘reflux’ or ‘backflow’ in the affected vein. A vein demonstrating reflux is termed ‘incompetent’.
There are three types of abnormal veins, which are frequently seen in combination. ‘Spider veins’ (telangiectasias) are the fine red capillary veins. The larger blue veins are called ‘reticular veins’, and are slightly deeper below the skin’s surface. Varicose veins are the largest of the abnormal veins, and may bulge above the skin’s surface.
Backflow from larger veins into smaller capillaries causes their distension and
the formation of so-called ‘spider veins’. This
is why treatment of spider veins in the presence of an underlying varicose vein
is not considered appropriate, because it does not address the underlying
problem. Backflow also leads to congestion of blood in the leg veins, which can
cause symptoms such as pain, fatigue, heaviness, aching, burning, throbbing,
cramping and restless legs. Symptoms are often made worse by prolonged standing.
The presence of a skin rash, small blue veins on the feet, skin discoloration
and ulcers usually indicate advancing vein problems. Severe varicose veins can
compromise the nutrition of the skin and lead to eczema, inflammation or even
ulceration of the lower legs. Treating the abnormal veins will lead to
improvement of the symptoms in the majority of patients.
Vein disorders are not always visible; diagnostic techniques are important
tools in determining the cause, severity and extent of the problem. Apart from
physical examination, non-invasive ultrasound is often used to assist with
assessment of the veins. Ultrasound investigation can accurately measure vein
diameter, assess reflux and contribute to a precise map of both normal and
abnormal veins of the leg.
WHAT CAUSES VARICOSE AND SPIDER VEINS?
A definitive cause is not known; however, a strong family history is a common
indication, suggesting that some patients inherit veins that are more likely to
deteriorate. Women are more likely to suffer from varicose veins at an earlier
age than men. Up to 30% of men and women are affected. In women, varicose veins
may worsen with fluctuations of hormones, such as during puberty, pregnancy and
menopause, and with the use of birth control pills. It is common for pregnant
women to develop varicose veins during the first trimester. Pregnancy results
in elevated hormone levels and blood volume, which in turn cause veins to
enlarge. In addition, the enlarging uterus causes increased pressure on the leg
veins. Varicose veins occurring in pregnancy will often improve significantly
within three months after delivery. However, with successive pregnancies,
abnormal veins are likely to get worse. Other predisposing factors include
ageing, standing occupations, obesity, lack of mobility, previous venous
thrombosis and leg injury.
DO WE NEED OUR VARICOSE AND SPIDER VEINS?
Varicose and spider veins are unhealthy superficial veins that do not function
correctly and fail to return blood back to the heart.
Varicose veins impose an extra burden on the deep veins, which can lead to
their deterioration. To compensate for the lack of function in varicose veins,
deep veins have to work harder, and in some cases, they become abnormal. Once
varicose veins are removed, the blood circulation will improve. In general,
varicose veins are not suitable for use in heart by-pass operations, because
they are damaged.
Spider veins are unsightly, abnormal veins and do not serve a biological
purpose.
WHEN DO YOU NEED TO TREAT YOUR VEINS?
Early treatment of varicose veins may reverse the symptoms of venous congestion
and minimise the risk of varicose vein-related complications and further
progression of the disease. Treatment becomes more urgent if there are
coexisting complications such as bleeding, inflammation (phlebitis), clots
(thrombosis), dermatitis or ulcers. In general, it is much easier to treat
varicose veins when they are smaller, as early treatment tends to be less
complicated and less involved. It is recommended that varicose veins be treated
before pregnancy, since complications such as clotting and bleeding can develop
during pregnancy. Varicose veins that have worsened during pregnancy may not
fully recover after pregnancy, requiring more involved and complicated
treatment than would have been required before pregnancy. Spider veins should
be treated only after the varicose veins have been successfully treated.
INVESTIGATIONS
Duplex Ultrasound Vein mapping
Before treating varicose veins, duplex ultrasound studies are organised to map
the abnormal veins.
Duplex Ultrasound is a specialised ultrasound, which shows the incompetent deep
and superficial veins. It also reveals any clots in the superficial and deep
veins. Deep vein thrombosis (DVT) scans may also be required if there is a history
of clotting. Patients with concurrent arterial disease may need additional
ultrasound studies to assess their arterial blood supply. Once tests are
completed, the phlebologist will be able to determine the most appropriate
course of treatment.

TREATMENT OPTIONS
Direct Vision Sclerotherapy
Direct Vision Sclerotherapy involves injecting a
sclerosing agent into abnormal surface veins using a fine needle. This
procedure is usually reserved for the treatment of small, blue superficial
veins (reticular veins), spider veins and sometimes for small visible varicose
veins. Successfully treated veins will fade as the body gradually removes them.
In many patients, sclerotherapy can relieve the symptoms caused by varicose
veins. With this procedure, veins can be dealt with at an earlier stage,
helping to prevent further complications.
Some veins may need to be injected more than once for optimum results.
Generally, normal activities can be resumed straight after sclerotherapy.
Medically prescribed compression stockings are essential to achieving the best
outcome, and may need to be worn for several days or weeks to assist in
resolution of the veins.
The procedure is performed in the doctor’s office and usually causes minimum,
transient discomfort. Microsclerotherapy is considered the gold standard in
treatment of spider veins of the legs.
Ultrasound Guided Sclerotherapy (UGS)
UGS is a modern technique that is reserved for
treating advanced varicose veins that are hidden beneath the skin. UGS is a
versatile procedure that can treat saphenous veins, perforating veins, and
other hidden varicose veins.
The ultrasound precisely displays the abnormal veins, as well as adjacent
structures such as deep veins and arteries. With ultrasound guidance, the
phlebologist can inject the hidden abnormal veins while observing the process
on the ultrasound monitor. Once injected, the treated vessel will be gradually
absorbed by the body and will disappear with time. A number of injections will
be required along the length of the vein to achieve complete closure. Another
significant advantage of this method is that it allows the phlebologist to
monitor the effect of each injection, while ensuring the safety of all adjacent
structures. The use of sclerosant as foam, rather than solution, has made this
procedure much more effective.
The treatment may take up to half an hour. Following the procedure, patients
are fitted with graduated compression stockings and asked to go for a 30-40
minute walk to promote blood flow in the deeper veins.
Endovenous Radiofrequency Ablation (RFA)
Endovenous RF Ablation is the latest method for the treatment of large
saphenous veins that would previously have been subjected to surgical stripping
under general anaesthetic.
RFA involves a combination of Radiofrequency and ultrasound technology,
and does not require admission to hospital or general anaesthesia. Published
research of the technique performed on more than 1000 patients has shown a low
risk of complications and superior results when compared with surgery and UGS
(excellent results in over 90% of patients).
RFA is used to treat the main trunks of abnormal saphenous veins. A fine laser
fibre is inserted into the target vein, under local anaesthetic. Radiofrequency
energy is then delivered into the vein, causing the vein to collapse and seal
shut. Following the procedure, compression stockings are prescribed and a daily
walk is advised.
To treat the remaining abnormal branch veins, UGS or phlebectomy (see below)
may be required.
Endovenous Glue ablation
The most recent innovation in the treatment of varicose veins is the use of medical glue known as VenaSeal (cyanoacrylate) to physically shut down and seal the main defective vein.Once the vein has been glued shut, it will undergo a process of hardening (sclerosis) and will be gradually absorbed by the body. The procedure is minimally invasive.
VenaSeal is a treatment that involves the application of a Medical Grade ‘Superglue’ into the disease vein, that collapses and permanently seals the vein off. It is a quick, minimally invasive procedure that takes approximately 15 minutes in experienced hands.
Venaseal adhesive is a special type of medical super-glue referred to as a ‘Cyanoacrylate’. It is very carefully formulated in specially designed labs and has some unique properties when compared to other medical grade glues on the market.
- When it comes into contact with blood within the vein wall, it polymerises rapidly. What this means is that it rapidly seals the vein shut upon application, with minimal migration.
- It is very soft and elastic, so that it is undetectable by the patient after application.
- Has an “anti-microbial” effect against gram positive organisms.
- Has been shown to have no adverse long term effects.
The published success of the VenaSeal closure procedure is up to 98.9% (VeClose study), with far fewer complications than EVLA or surgery.
VenaSeal has been meticulously trialed in the United States and Europe over the last 5 years. Results published show a low risk of complications and excellent medium-term results. The VeClose study out of Germany, showed a 98.9% closure rate at 6 months. VenaSeal is considered as effective as endovenous laser ablation
Ambulatory Phlebectomy
Ambulatory phlebectomy is the surgical removal of superficial varicose veins.
This is usually done in the office, using local anaesthesia. Incisions are tiny
(stitches are generally not necessary) and scarring is minimal. After the vein
has been removed, a bandage and/or compression stockings are worn for a short
period of time.
Surgery
Surgical techniques include ligation (tying
off the vein), stripping (removal of an
extensive segment of vein by pulling it out) and phlebectomy (removal of veins through tiny
incisions). Surgery may be performed using local, spinal or general
anaesthesia, with most patients returning home the same day as the procedure.
Surgery has traditionally been used to treat large varicose veins, but recent
studies indicate a poor long-term success rate.
Vascular Lasers & Intense Pulse Light
These techniques have proved disappointing in treating spider veins of the leg.
Light-based treatment is generally only suitable for small veins above the
waist, and is best used to treat vascular lesions such as birth marks (such as
port-wine stains) and facial veins.
Sclerotherapy remains the gold standard for treatment of
superficial leg veins.
IMPORTANT GENERAL MEASURES
A number of simple measures should be followed to prevent further deterioration
of varicose veins.
1. Activate your calf muscles (by walking, jogging, running).
This will encourage the muscles to contract, which will stimulate blood flow
through the venous system and the return of blood back to the heart.
2. Elevate the legs when you can. This will help the
return of blood to the heart.
3. Wear graduated compression stockings. These provide
more compression near the ankles and less further up the limb, which encourages
the flow of blood back to the heart.
4. Avoid prolonged sitting and standing. Exercise activates
your calf muscles and helps to empty your veins. When sitting or standing
cannot be avoided, activate the calf muscle pump by flexing your feet, to lift
your heels off the ground. At work or during long distance travel, get up from
time to time and go for a walk.
5. Lose weight. Excess weight can worsen varicose veins
and cause both venous and lymphatic problems.
WHAT ARE THE POSSIBLE COMPLICATIONS IF I DO NOT HAVE ANY
TREATMENT?
- With large varicose veins, spontaneous blood clots may develop in the superficial veins and, more rarely, in the deep veins. Clots in the deep veins (deep vein thrombosis or DVT) can dislodge and travel to the lungs, which can cause pulmonary embolism; a life-threatening condition.
- Skin changes, including increased or decreased pigmentation, hardening of the skin and underlying fat (lipodermatosclerosis)
- Ulcers may develop in later stage. Ulcers may become weepy, infected and painful, and take longer to heal.
- If the varicose veins are injured by accident, it can cause uncontrolled bleeding because of incompetent veins.
- Spider veins may indicate an underlying varicose vein disease, but otherwise are mainly a cosmetic concern.
Complications of Varicose vein treatment
Common Complications
- Pain – at the injection site due to inflammation (Thrombophlebitis)
- Bruising – Due to extravasation of blood.
- Localised hives – due to allergic reaction
- Small superficial ulcers – due to localised skin necrosis
- Hyperpigmentation – staining of skin due to iron pigments liberated from clotted blood in the sclerosed veins
Rare Complications
- Migraine attacks – commonly those who have persistent hole in the septum between 2 heart chambers
- Stroke/Ministroke – Due to air embolus passing to the brain
- DVT – Deep Vein Thrombosis
- Pulmonary embolism – Clots from DVT travelling to the lungs
Vein Information – Download
Pre-Post Vein Treatment Instructions – Download